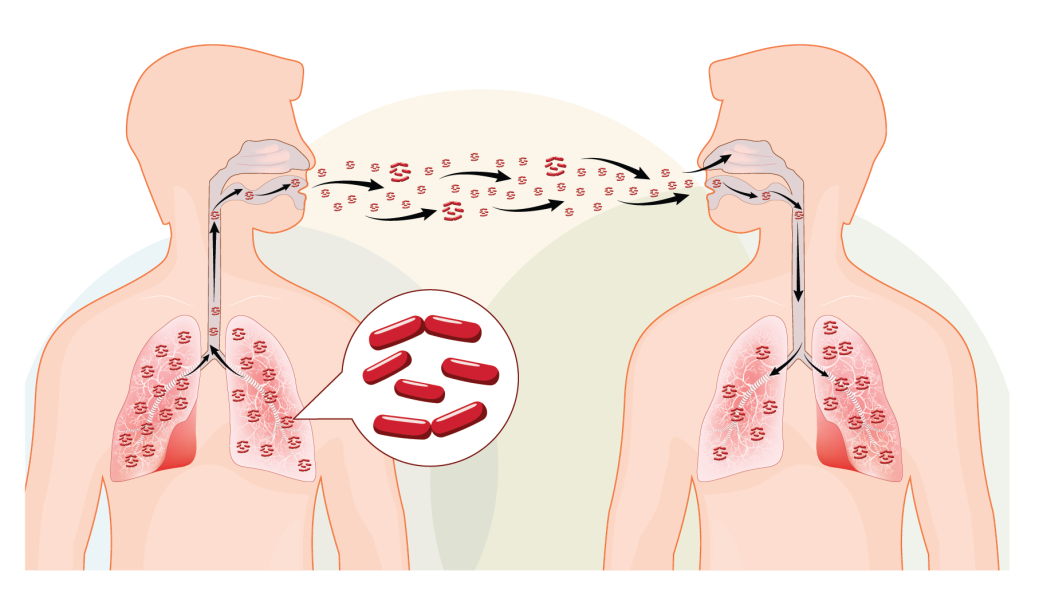
Tubercolosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis. It primarily affects the lungs but can also affect other parts of the body. TB is a contagious disease, but it’s not easily caught. It spreads through the air when an infected person coughs, sneezes, or talks, releasing tiny infectious droplets into the air.
Here are some key points about Tuberculosis:
- Transmission: TB is mainly spread through the inhalation of airborne droplets containing the bacteria. Close and prolonged contact with an infected person is usually required for transmission.
- Not Highly Contagious: TB is considered less contagious compared to some other respiratory infections. Casual contact, such as brief interactions or touching surfaces, is unlikely to result in transmission.
- Symptoms: The symptoms of TB include persistent cough, chest pain, weight loss, fatigue, fever, and night sweats. Latent TB infection may have no symptoms.
- Testing: Testing for TB includes skin tests, blood tests, chest X-rays, and sputum tests. It’s important to diagnose and treat TB promptly to prevent its spread.
- Treatment: TB is treatable with a course of antibiotics. Completing the entire course of medication is crucial to prevent drug-resistant strains from developing.
- Prevention: Prevention strategies include identifying and treating active cases promptly, vaccination (BCG vaccine), and implementing infection control measures in healthcare settings.
While TB is a serious infectious disease, it is not as easily transmitted as some other respiratory infections. Early detection, proper treatment, and public health measures play essential roles in controlling its spread. If someone is experiencing symptoms of TB or has been in contact with an infected individual, it is important to seek medical advice promptly.
Who is at risk of having active Tuberculosis?
Not everyone infected with the tuberculosis (TB) bacteria develops active TB disease. In many cases, the immune system is able to contain the bacteria, leading to latent TB infection. However, certain factors increase the risk of progressing from latent TB to active TB disease. Individuals at higher risk for developing active TB include:
- People with Weakened Immune Systems: Individuals with weakened immune systems are at a higher risk of developing active TB. This includes people living with HIV/AIDS, those undergoing chemotherapy, organ transplant recipients, and individuals on immunosuppressive medications.
- Recent TB Infection: If someone has been recently infected with TB bacteria, their risk of developing active TB is higher than those with longstanding latent TB infection.
- Infants and Young Children: Children, particularly those under the age of 5, are at an increased risk of developing active TB if they are infected.
- Elderly Individuals: Older adults, especially those over the age of 65, may be more vulnerable to developing active TB.
- Certain Medical Conditions: People with certain medical conditions such as diabetes, chronic kidney disease, and malnutrition may be more susceptible to developing active TB.
- Substance Abuse: Individuals who misuse substances, especially intravenous drug users, have an increased risk of developing active TB.
- Close Contacts of Active TB Cases: People who have close and prolonged contact with someone diagnosed with active TB are at an elevated risk.
- Underlying Lung Disease: Individuals with conditions that affect the lungs, such as silicosis or previous TB scarring, are at a higher risk.
It’s important to note that latent TB infection does not transmit the disease to others. Active TB, on the other hand, is contagious, and individuals with active TB need prompt treatment to prevent the spread of the disease. If someone falls into one of the high-risk categories or experiences symptoms such as persistent cough, chest pain, weight loss, fatigue, fever, or night sweats, they should seek medical attention for testing and evaluation.
How can I tell if I have TB?
Tuberculosis (TB) can present with a variety of symptoms, and it’s important to be aware of them, especially if you fall into high-risk groups or have been in contact with someone diagnosed with active TB. Common symptoms of tuberculosis include:
- Persistent Cough: A cough that lasts for more than three weeks is one of the hallmark symptoms of TB. The cough may produce phlegm or blood.
- Chest Pain: Pain or discomfort in the chest may be experienced, especially during coughing or breathing.
- Coughing up Blood: Hemoptysis, or coughing up blood, can occur in more advanced cases of TB.
- Weight Loss: Unintentional weight loss is a common symptom of active TB.
- Fatigue: Persistent fatigue and weakness may be present.
- Fever: Low-grade fever, especially in the afternoon or evening, is a possible symptom.
- Night Sweats: Profuse sweating during the night is a characteristic symptom of TB.
- Loss of Appetite: A decreased appetite leading to weight loss is common.
- Shortness of Breath: Difficulty breathing or shortness of breath may occur, particularly as the disease progresses.
It’s important to note that not everyone infected with the TB bacteria develops symptoms. In some cases, the infection remains latent, meaning the bacteria are present but not causing illness. If you suspect you may have TB, especially if you exhibit any of the symptoms mentioned above, it’s crucial to seek medical attention promptly. TB is a treatable and curable disease with appropriate medications, but early detection and treatment are key to preventing the spread of the disease to others.
Medical professionals can conduct tests such as a chest X-ray, sputum culture, and tuberculin skin test to diagnose TB. If you have been in contact with someone diagnosed with active TB or if you are experiencing symptoms, contact your healthcare provider for an evaluation.
What are the TB treatments?
The treatment for tuberculosis (TB) typically involves a course of specific antibiotics to kill the bacteria causing the infection. The most commonly used drugs for TB treatment are isoniazid, rifampin, ethambutol, and pyrazinamide. The specific combination and duration of these drugs depend on factors such as the type of TB, drug resistance, and individual patient circumstances.
Here is a general overview of TB treatment:
- First-Line Drugs:
- Isoniazid (INH): Often a key component of TB treatment, isoniazid kills actively dividing bacteria.
- Rifampin (RIF): Another essential drug, rifampin works to eliminate TB bacteria, including those that may be resistant to isoniazid.
- Ethambutol (EMB): This drug is effective against TB bacteria and is often used in combination with isoniazid and rifampin.
- Pyrazinamide (PZA): Pyrazinamide is used during the initial phase of treatment and helps to eliminate TB bacteria.
- Treatment Duration:
- The initial phase of TB treatment usually lasts for 2 months, during which a combination of isoniazid, rifampin, ethambutol, and pyrazinamide is prescribed.
- After the initial phase, the continuation phase follows, typically involving isoniazid and rifampin for 4 to 7 months.
- Directly Observed Therapy (DOT):
- TB treatment often involves Directly Observed Therapy, where a healthcare provider or another designated person ensures that the patient takes the prescribed medications.
- Monitoring and Follow-up:
- Regular monitoring and follow-up are essential to assess treatment progress and address any side effects or complications.
- Drug susceptibility testing may be performed to determine if the TB bacteria are resistant to certain medications.
It’s crucial for individuals undergoing TB treatment to complete the entire course of medications as prescribed by their healthcare provider, even if symptoms improve before the course is finished. Incomplete treatment can lead to the development of drug-resistant TB.
TB treatment is highly effective when followed as prescribed, and most individuals can recover fully with proper medical care. If you suspect you have TB or have been diagnosed, it’s important to work closely with your healthcare provider to initiate and complete the appropriate treatment regimen.
Is there a TB vaccine available?
Yes, there is a vaccine for Tuberculosis (TB) known as the Bacille Calmette-Guérin (BCG) vaccine. The BCG vaccine is named after the French scientists who developed it, Albert Calmette and Camille Guérin. It is the only licensed vaccine for TB.
Here are key points about the BCG vaccine:
- Purpose:
- The BCG vaccine is primarily used to prevent severe forms of TB in children, particularly TB meningitis and disseminated TB.
- Effectiveness:
- The BCG vaccine is more effective in preventing severe forms of TB in children than in preventing pulmonary TB in adults. Its effectiveness can vary based on factors such as geographic location and the prevalence of different strains of TB.
- Not a Guarantee Against All Forms of TB:
- The BCG vaccine does not provide complete protection against all forms of TB. It is not very effective in preventing pulmonary TB in adults, which is the most common form of the disease.
- Timing of Vaccination:
- The BCG vaccine is typically administered to infants in countries with a high prevalence of TB. The timing of administration can vary, but it is often given shortly after birth.
- Revaccination:
- There is ongoing research on the potential benefits of revaccination with BCG, particularly in areas with a high burden of TB.
- TB Testing and BCG Vaccination:
- BCG vaccination can affect the interpretation of certain TB diagnostic tests, such as the tuberculin skin test (TST) and interferon-gamma release assays (IGRAs). This can complicate the diagnosis of TB infection in vaccinated individuals.
It’s important to note that while the BCG vaccine plays a role in TB prevention, it is not a substitute for comprehensive TB control measures, including early diagnosis and appropriate treatment of active TB cases.
The BCG vaccine is widely used in many countries, but its effectiveness and recommendations for use may vary based on regional factors and national guidelines. If you have specific concerns or questions about TB vaccination, it is advisable to consult with healthcare professionals or public health authorities in your area.




